Atypical Presentations of Pilonidal Sinus Disease: A Case Series with Literature Review
Abstract
Introduction: Pilonidal sinus (PNS) typically arises in the sacrococcygeal region but can occasionally present in atypical locations, including the axilla, intermammary region, umbilicus, interdigital web, and neck, often leading to delayed diagnosis and suboptimal management. This study aims to examine clinical features, surgical management, and outcomes of PNS in these uncommon sites.
Methods: This retrospective case series was conducted at a single center over eight years and examined patients with extra-sacrococcygeal PNS confirmed by histopathology. Clinical, surgical, and follow-up data were retrieved from patient records. Data were analyzed using SPSS 25.0 and presented as descriptive statistics (frequencies, percentages, means, and ranges).
Results: This study included 4 patients, with an equal sex distribution (2 females, 50%; 2 males, 50%) and a mean age of 24 years (range: 16–31). Presenting symptoms included discharge, itching, pain, redness, and mass formation. None had significant past medical history, and one patient (25%) had prior surgery at the same site. Affected sites were equally distributed: breast (25%), axilla (25%), penile (25%), and scalp (25%). All patients underwent surgical intervention, and histopathology revealed tracts lined with epidermis, surrounded by mixed inflammatory cells, foreign body giant cells, and hair shafts in granulation tissue. During the follow-up period (mean follow-up: 13.5 months), no recurrence was observed.
Conclusion: Atypical presentations of PNS, although rare, can occur in diverse anatomical regions. Surgical excision with primary closure might be an effective treatment approach, potentially leading to favorable clinical outcomes and a low recurrence rate.
Introduction
Pilonidal sinus (PNS) is a common inflammatory disorder that typically occurs in the natal cleft, resulting from hair penetration into the skin, forming a tract lined with granulation tissue, which may develop into a pus-filled cavity [1,2]. The condition was first described by Mayo in 1833, who identified a hair-containing cyst just below the coccyx. The term "pilonidal" was coined by Hodge in 1880 and is derived from its Latin roots. Despite being recognized for nearly two centuries, the pathogenesis of PNS remains a subject of ongoing debate [3]. Notable contributions by Karydakis and Bascom have shifted the understanding of PNS from a congenital neural tube abnormality to an acquired condition, emphasizing the role of environmental and lifestyle factors [4,5]. PNS risk factors include poor hygiene, a deep natal cleft, excessive hair growth, and a sedentary lifestyle. Although often asymptomatic, PNS may present as a recurrent abscess or a non-healing draining sinus [4]. The condition predominantly affects the sacrococcygeal area of hirsute males, with an estimated incidence of 26 per 100,000 people [6]. However, in rare cases, PNS can develop in atypical locations, including the axilla, intermammary region, umbilicus, interdigital webs, occiput, scalp, endoanal canal, groin, suprapubic area, clitoris, penis, and prepuce [2,3,7].
Given the scarcity of literature on atypical presentations of PNS, the current study aims to examine the clinical features and management of PNS in atypical locations (extra-sacrococcygeal). The eligibility of the references has been confirmed [8].
Methods
Study Design
This retrospective case series was conducted over eight years at a single private facility, focusing on patients with atypical PNS who were evaluated, treated, and followed up. Ethical approval for this study was obtained from the Ethical Committee of the Kscien Organization (Approval No. 31/2025). Clinical, surgical, and follow-up data were collected through a systematic review of electronic medical records, surgical pathology reports, and consultation with treating healthcare providers when necessary. Informed consent was obtained from all patients or their guardians for the publication of their anonymized data.
Setting and Participants
The study included patients with atypical (extra-sacrococcygeal) PNS presentations who were admitted to the hospital during the study period. Clinical and sociodemographic data were collected from patient records. The following variables were recorded: age, gender, signs and symptoms, past medical and surgical history, clinical examination findings, ultrasound (US) findings, surgical indications, type of surgery performed, histopathological results, complications, and follow-up duration.
Inclusion and Exclusion Criteria
Eligible participants were those with confirmed PNS diagnoses through HPE. Patients with incomplete clinical or sociodemographic data or those whose diagnosis could not be confirmed through histopathology were excluded. Patients with primary sacrococcygeal PNS or those lacking follow-up data were also excluded from the study.
Surgical Management
All patients underwent thorough preoperative planning and assessments to evaluate their suitability for local anesthesia. Preoperative evaluations included US, monitoring of vital signs, viral screening, and hematological assessment, including a complete blood count and hemoglobin level measurement. Surgical procedures were performed with patients in the supine position. The surgical approach involved wide local excision of the PNS followed by primary closure. Following wide local excision, Salih’s preparation (a mixture of sclerosing agent and Lawsonia inermis) was applied to the wound bed and sinus margins prior to primary closure. This was performed to enhance wound healing and reduce the risk of infection [9]. Postoperative pain was managed with oral paracetamol at a dose of 1,000 mg, administered every 6–8 hours as needed, for a minimum of five days.
Statistical Analysis
The data were organized and analyzed using Microsoft Excel 2019. Descriptive analysis was conducted using the Statistical Package for Social Sciences (SPSS) version 25.0. The results are presented as frequencies, percentages, means, and ranges.
Results
Clinical and Histopathological Features
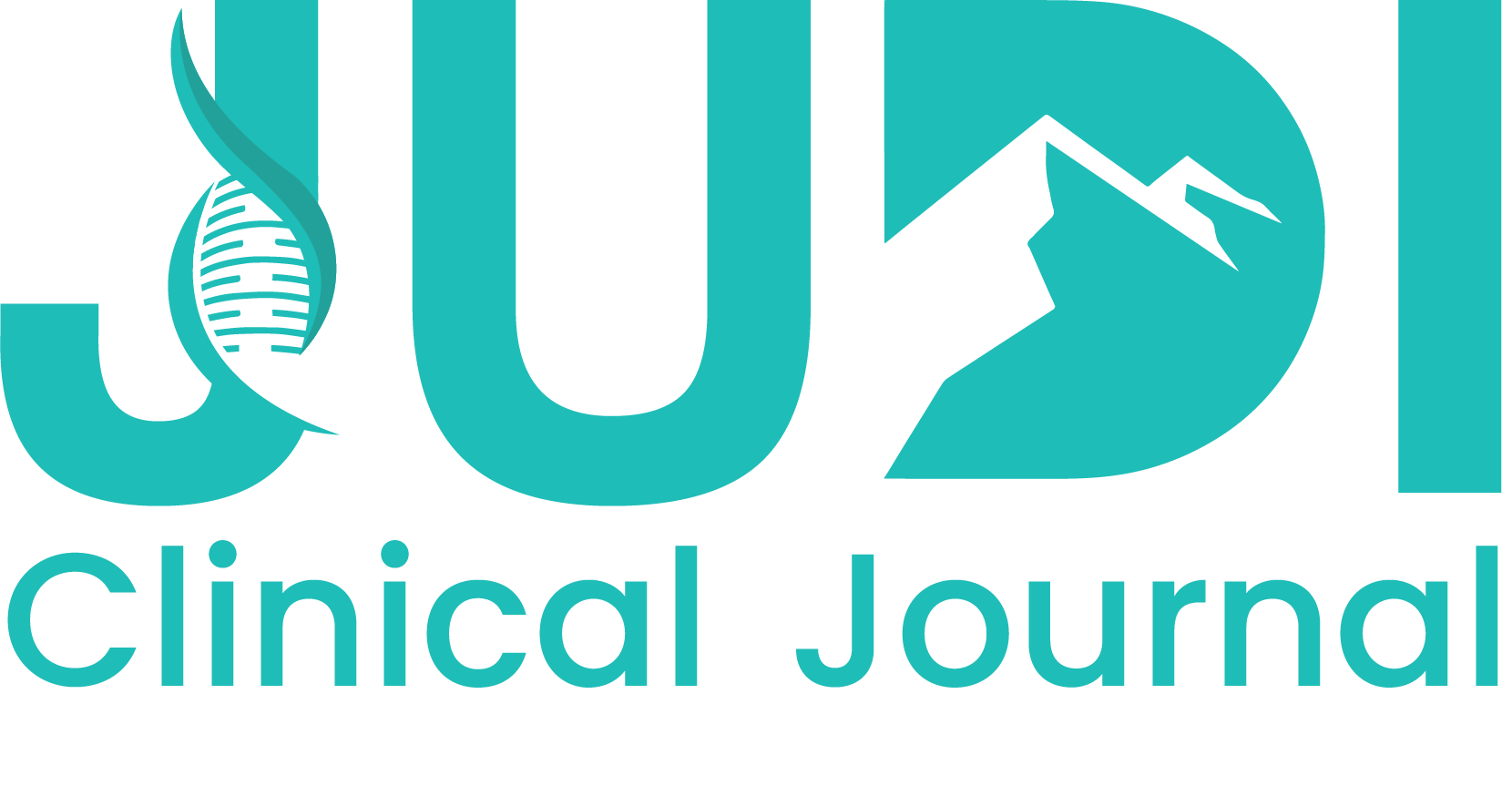
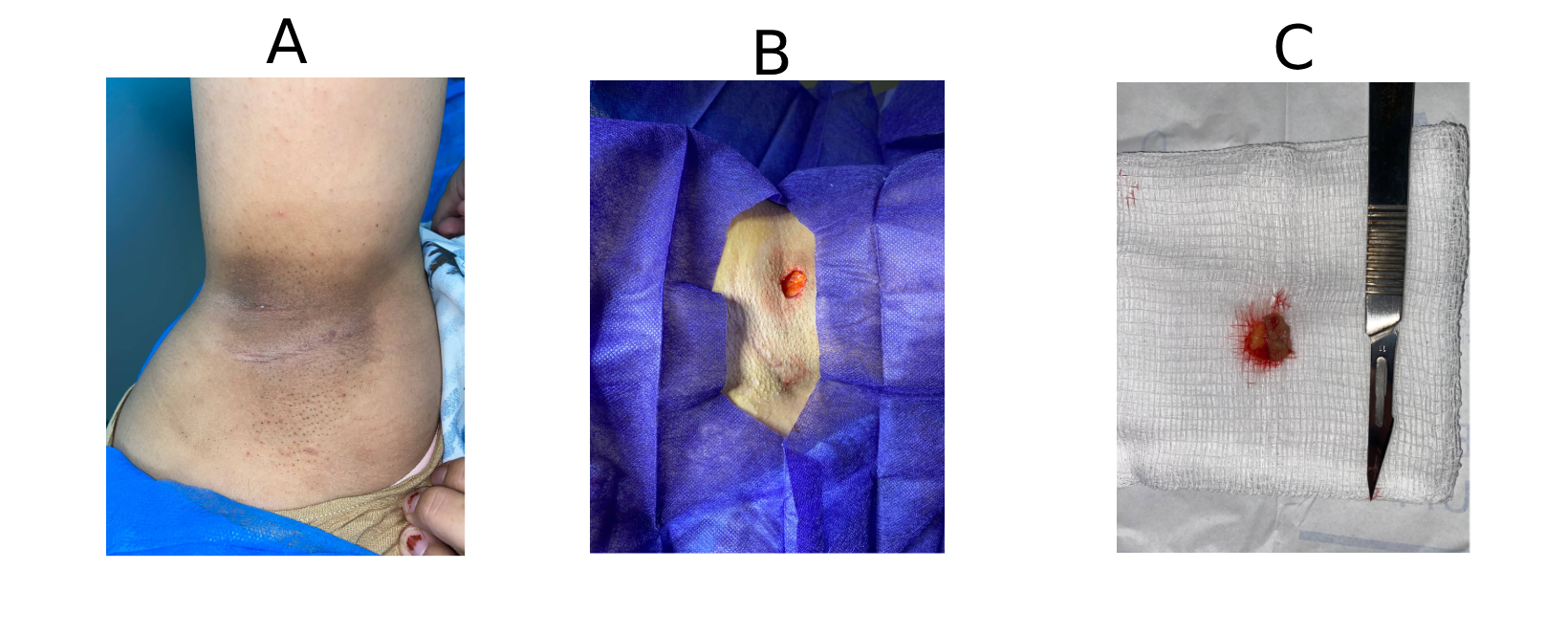
This study included four patients, comprising 2 females (50%) and 2 males (50%), with a mean age of 24 years (range: 16–31 years) (Table 1). Patients presented with various symptoms, including discharge, itching, pain, and erythema. None of the patients had significant past medical history. One patient (25.0%) had a history of prior surgery at the same site. The affected sites varied, with the breast, axilla, penile, and scalp region each in one case (Figures 1 and 2). Ultrasound imaging was performed in three of four cases (75%), and the findings revealed simple breast cysts with associated midline and inframammary PNS, infected dermal–subdermal cysts with mild edema, and chronic PNS in the left temporal scalp region (Table 1). All patients underwent surgical intervention, including excision of sinuses or complete removal of masses/nodules. HPE revealed tracts lined with epidermis, surrounded by mixed inflammatory cells, foreign body giant cells, and hair shafts embedded in granulation tissue.
|
Case / Authors [Ref] |
Age (Y) |
Sex |
Sign & Symptoms |
Location |
PMH |
PSH |
Examination Findings |
Imaging (US) |
Surgical Indication |
Type of Surgery |
Histopathology |
Follow-Up |
|
Salih & Kakamad [2] |
39 |
M |
Perianal discharge and pruritus |
Endoanal |
Negative |
Surgically treated PNS and anal fistula |
External opening at 11 o’clock, 3.5 cm from anal verge with induration and surrounding excoriation |
Single fistulous tract extending into anal canal |
Discharge and pain during defecation |
Fistulectomy |
Chronic inflammation with scattered foreign body giant cells consistent with PNS |
Symptom-free at 5 weeks |
|
Salih & Kakamad [3] |
19 |
M |
Chronic nodule |
Scalp |
Negative |
Negative |
2×2 cm mobile nodule in left parieto-occipital region with central punctum |
Not performed |
Intermittent discharge |
Complete excision |
Mixed inflammatory cells with foreign body giant cell reaction containing hair |
No recurrence at 3 months |
|
Salih et al. [7] |
22 |
F |
Painful submental mass |
Submental |
Negative |
Operation at same site 6 years prior |
Tender 2×2 cm mass attached to skin, no external opening |
Well-defined hyperechoic lesion suggestive of dermoid cyst |
Painful mass |
Complete excision |
Mixed inflammatory cells with foreign body giant cell reaction containing hair |
No recurrence at 2 years |
|
Salih et al. [10] |
27 |
M |
Painless postauricular discharge |
Auricle |
Negative |
Negative |
NA |
Not performed |
Discharge |
Excision of sinuses |
NA |
No recurrence |
|
Salih et al. [11] |
25 |
F |
Bilateral Multiple discharging sinuses |
Breast |
Negative |
Negative |
Multiple discharging sinuses with induration and tenderness |
Not performed |
Discharge |
Excision of sinuses |
Chronic foreign body granuloma surrounding hair |
No recurrence at 6 months |
|
Salih & Kakamad [12] |
22 |
M |
Pain and purulent discharge |
Auricle |
Negative |
Negative |
2 cm scar with single central opening |
Not performed |
Pain and discharge |
Complete excision |
Mixed inflammatory cells with foreign body giant cell reaction containing hair |
No recurrence |
|
Salih et al. [13] |
20 |
F |
Yellowish discharge |
Neck |
Negative |
Negative |
10 openings on nape, 7×4 cm induration and erythema |
Not performed |
Multiple sinuses with discharge |
Excision of sinuses |
Free hair shaft embedded within chronic inflammation and granulation tissue |
Healthy at 2 months |
|
Salih et al. [14] |
35 |
F |
Discharging lesion |
Breast |
Negative |
Negative |
Local redness with multiple discharging sinuses, 3–4 cm from nipple |
Not performed |
Remission and relapse |
Excision of sinuses |
Hair shaft surrounded by granulation tissue |
No recurrence at 6 months |
|
Salih et al. [15] |
22 |
F |
Pain, discharge, and erythema |
Breast |
Negative |
Negative |
Single sinus with clear discharge, surrounding old scar |
Not performed |
Discharge |
Wide local excision |
Inflammatory reaction and foreign body giant cells surrounding hair shaft |
No recurrence |
|
Salih et al. [16] |
16 |
F |
Chronic discharging sinus |
Breast |
NA |
Negative |
Single discharging sinus, 8×9 cm induration |
Not performed |
Discharge |
Excision of sinuses |
Inflammatory cell collection with pus and scattered hair shafts |
No recurrence at 4 months |
|
Salih et al. [17] |
25 |
M |
Mass with chronic discharge |
Auricle |
Negative |
Negative |
1×1 cm firm, tender nodule attached to skin |
Not performed |
Discharge |
Mass excision |
PNS |
No recurrence at 8 months |
|
Present study (Case 1) |
31 |
F |
Intermammary mass with erythematous nodules |
Breast |
Negative |
Negative |
Midline swelling without ulceration or discharge |
Simple breast cysts with midline and inframammary PNS |
Painful mass |
Complete excision |
Mixed inflammatory cells with foreign body giant cell reaction containing hair |
No recurrence at 4 years |
|
Present study (Case 2) |
27 |
F |
Right axillary mass, 4-year duration |
Axilla |
Negative |
Negative |
Linear scar with mild hyperpigmentation, chronic PNS |
Infected dermal-subdermal cysts with mild edema |
Painful mass |
Excision of sinuses |
Mixed inflammatory cells with foreign body giant cell reaction containing hair |
No recurrence at 1 month |
|
Present study (Case 3) |
22 |
M |
Perianal discharge and pruritus |
Penile |
Negative |
Negative |
Linear scar, chronic PNS without active inflammation |
NA |
Sinus |
Excision of sinus |
PNS |
No recurrence at 2 months |
|
Present study (Case 4) |
16 |
M |
Painless scalp discharge |
Scalp |
Negative |
Skin laceration at same site |
NA |
Left temporal scalp chronic PNS |
Sinus |
Excision of sinus |
PNS |
No recurrence at 3 months |
|
F: Female, M: Male, PMH: past medical history, PSH: past surgical history, PNS: pilonidal sinus, US: ultrasound, NA: not available, Y: Years |
||||||||||||
Outcomes and Follow-up
All 4 cases had favorable outcomes with no recurrence. Follow-up duration ranged from 1 month to 4 years, with the mean follow-up period being 13.5 months. No significant complications or adverse events occurred, and postoperative recovery was uneventful, with no need for further interventions.
Discussion
The pilonidal disease has a spectrum of clinical manifestations, ranging from asymptomatic to large, symptomatic abscesses. The exact cause of PNS remains unclear, with two main theories, acquired and congenital, offering potential explanations for its development. The formation of PNS generally requires three key factors: the presence of hair in the skin, a region of wrinkled skin (such as the natal cleft or a scar), and a combination of hormonal and hygiene-related factors [5]. This condition is less frequent before puberty and after the age of 40 years, likely due to the influence of sex hormones during these periods. It is also three times more common in males than females. Studies have shown that individuals who sit for prolonged periods and bathe less frequently are at a significantly higher risk of developing PNS, with a 219-fold increased risk compared to those without these risk factors [2,10]. Among the 11 cases reported in the literature, the mean patient age was 24.7 years (range: 16–39 years). The most commonly affected site was the breast (36.4%), followed by the auricle (27.3%), with single cases involving the endoanal, scalp, submental, and neck regions (each 9.1%). The sex distribution showed a slight male predominance, with 6 males (54.5%) and 5 females (45.5%) (Table 1) [2,3,7,10–17]. In line with these findings, the current case series included 4 patients with an equal sex distribution (2 males, 50%; 2 females, 50%) and a comparable mean age of 24 years (range: 16–31 years).
The differential diagnosis for atypical PNS includes a broad range of conditions, such as hernia, endometriosis, urachal cyst, pyogenic granuloma, epidermoid cyst, dermoid cyst, and infected sebaceous cyst. Clinical signs often include pain, warmth, and swelling, indicating inflammation. This condition is multifaceted, causing physical discomfort and emotional distress for those affected, leading to direct healthcare costs and indirect societal costs due to lost work hours [11,12]. Among the cases reviewed, the most common presenting symptom was discharge (9/11, 81.8%), followed by pain (3/11, 27.3%) and mass or nodule formation (2/11, 18.2%) [2,3,7,10–17]. In the current series, two (50%) presented with masses (intermammary and axillary), and two (50%) presented with discharge (perianal and scalp), with pruritus, erythema, painless presentation, and chronicity each observed in a single case (25%).
PNS is most commonly diagnosed based on the clinical presentation, with laboratory or radiologic investigations generally unnecessary [10]. However, US can reveal strands of hair associated with the lesion. Fine needle aspiration cytology can help to rule out a neoplastic process, particularly when the suspicion for PNS disease is low [10]. Ultrasonography was performed in only 2 of the 11 cases reviewed (18.2%). One case demonstrated a single fistulous tract extending into the anal canal, while another revealed a well-defined hyperechoic lesion suggestive of a dermoid cyst. In the remaining 9 cases (81.8%), ultrasound evaluation was not carried out [2,3,7,10–17]. In the current series, ultrasound was performed in three of four cases (75%). Findings included simple breast cysts with associated midline and inframammary PNS, infected dermal–subdermal cysts with mild edema, and chronic PNS in the left temporal scalp region
A variety of both surgical and non-surgical approaches are utilized in managing PNS. Surgical interventions include simple incision and drainage, marsupialization, open wound management, primary closure, and rhomboid excision followed by a Limberg flap. Non-surgical methods typically involve the injection of sclerosing and wound-enhancing agents into the sinus tract. Managing atypical PNS often necessitates more tailored approaches, such as resection with or without primary closure. Postoperative complications and recurrences are common, with significant risk factors identified, including obesity, a family history of PNS, male sex, tobacco use, inadequate hygiene, sinus size, and the specific surgical technique employed [3, 4]. The ideal management of PNS should aim to alleviate patient discomfort, reduce hospital stays, minimize recurrence rates, address complications, and limit prolonged work absences [4].
Furthermore, the treatment should be safe, effective, and free from adverse consequences. Surgical approaches, however, may not align with these optimal treatment goals, as they can result in discomfort and prolonged work absences. While surgery remains the recommended approach for atypical PNS, it also facilitates a definitive diagnosis through HPE. Shareef et al. conducted a study involving 12 female patients, all presenting with discharge lasting from four weeks to two years. Nine of these patients underwent resection with direct closure, without a flap, while the remaining three had their PNS excised and allowed to heal secondarily. Recurrence was observed in three of the patients [13-18]. Among the cases reviewed, excision of sinuses was the most commonly performed procedure (5/11, 45.5%), followed by complete excision (3/11, 27.3%). Fistulectomy, wide local excision, and mass excision were each performed in a single case (9.1%) [2,3,7,10–17]. In the current series, surgical management included excision of a single sinus in two cases (50%), complete excision in one case (25%), and excision of multiple sinuses in one case (25%). All 15 cases, including 11 reviewed in the literature and 4 from the current series, remained symptom-free with no recurrence during follow-up.
This study has several limitations. First, the retrospective design may introduce selection bias and limit the ability to establish causal relationships. Second, the small sample size limits the generalizability of the findings. Third, the follow-up period varied among the patients, which could affect the assessment of long-term outcomes. Finally, the study was conducted at a single center, which may not reflect the broader population.
Conclusion
This case series highlights the rare occurrence of PNS in atypical locations, with clinical and HPE findings that resemble typical cases. Surgical excision might result in favorable outcomes without recurrence.
Declarations
Conflicts of interest: The authors have no conflicts of interest to disclose.
Ethical approval: Ethical approval was obtained from the Ethical Committee of the Kscien Organization (Approval No. 31/2025)
Consent for participation: Not applicable.
Consent for publication: Informed consent was obtained from all patients or their guardians for the publication of their anonymized data.
Funding: The present study received no financial support.
Acknowledgements: None to be declared.
Authors' contributions: SL, HHK, DAI, and AMM: Major contributors to the conception of the study, as well as the literature search for related studies, and manuscript writing. KMS, SHH, KAN, HAA, AAQ and AMA: Literature review, critical revision of the manuscript, and processing of the tables and figures. All authors have read and approved the final version of the manuscript.
Use of AI: ChatGPT-4.5 was used to assist with language refinement and improve the overall clarity of the manuscript. All content was thoroughly reviewed and approved by the authors, who bear full responsibility for the final version.
Data availability statement: Not applicable.
References
- Salih AM, Rahim HM, Abdalla BA,Kakamad FH, Mhamad UA, Ahmed GS, et al.Trial of induction of pilonidal sinus disease in a rat model; An Animal Study. Barw Medical Journal.2023Jan30;1(1):2-4. doi:10.58742/bmj.v1i1.9
- Salih AM, Kakamad FH. A case report of endoanal pilonidal sinus. Journal of Case Reports and Images in Surgery. 2016:60-62. doi:10.5348/Z12-2016-24-CR-16
- Salih AM, Kakamad FH. Scalp pilonidal sinus: A case report. International Journal of Case Reports and Images (IJCRI). 2016,1;7(3):175-177.doi:10.5348/ijcri-201629-CR-10616
- Tam A, Steen CJ, Chua J, Yap RJ. Pilonidal sinus: an overview of historical and current managementmodalities. Updates in Surgery. 2024,76(3):803-10. doi:10.1007/s13304-024-01799-2
- Noviello C, Romano M, Marzuillo P, Andrea R, Papparella A. Unusual position of pilonidal sinus in children may explain its malformative etiology: Case report and review of the literature. International Journal of Surgery Case Reports. 2024; 116:109444. doi:10.1016/j.ijscr.2024.109444.
- Chirila DN, Pop TR, Gligor D, Chirila MD. Unusual site of a pilonidal cyst. Human and Veterinary Medicine. 2017, 9(3):76-78.
- Salih AM, Kakamad F, Habibullah IJ, Abdulqadr MH. Submental pilonidal sinus-the first reported case. Pilonidal Sinus J. 2017, 3(1):14-18.
- Abdullah HO, Abdalla BA, Kakamad FH, Ahmed JO, Baba HO, Hassan MN, et al. Predatory Publishing Lists: A Review on the Ongoing Battle Against Fraudulent Actions. Barw Med J. 2024;2(2):26-30. doi:10.58742/bmj.v2i2.91
- Salih AM, Kakamad FH, Salih RQ, Mohammed SH, Habibullah IJ, Hammood ZD, et al. Nonoperative management of pilonidal sinus disease: one more step toward the ideal management therapy—a randomized controlled trial. Surgery. 2018;164(1):66-70. doi:10.1016/j.surg.2017.12.014
- Salih AM, Hassan SH, Hassan MN, Fatah ML, Kakamad FH, Salih BK, Mohammed SH. Auricular pilonidal sinus; a rare case with a brief review of literature. International Journal of Surgery Open. 2022,1; 43:100489. doi:10.1016/j.ijso.2022.100489
- Salih AM, Mohammed SH, Mustafa MQ, Essa RA, Kakamad FH, Mikael TM, Omar DA, Mohammed KK, Hassan HA, Aziz MS, Usf DC. Bilateral inframammary pilonidal sinus: a case report with literature review. International Journal of Surgery Case Reports.2020;67:18-20. doi:10.1016/j.ijscr.2020.01.003
- Salih AM, Kakamad FH. Preauricular pilonidal sinus: the first reported case. Int J Case Rep Images.2016, 1;7(3):162-164. doi:10.5348/ijcri-201626-CR-10613
- Salih AM, Kakamad FH, Salih RQ, Baba HO, Mohammed SH, Najar KA, Kakamad SH, Abdullah AN. Pilonidal sinus of neck: A case report. Int J Case Rep Images. 2018;9:100882Z01AS2018. doi:10.5348/100882Z01AS2018CR
- Salih AM, Kakamad FH, Hammood ZD, Baba HO, Habibullah IJ, Salih RQ, Mohammed SH. Pilonidal sinus of breast: A case report with literature review. International Journal of Surgery Case Reports.2019, 66(2020):204-206. doi:10.1016/j.ijscr.2019.11.057
- Salih AM, Kakamad F, Baba HO, Mohammed SH, Hussein DA, Ahmmad DR, Othman S, Rahim HM. Recurrent intermammary pilonidal sinus: a rare case with literature review. Pilonidal Sinus Journal.2018, 4(1):13-18.
- Salih AM, Kakamad FH, Abdulqadr MH. Intermammary pilonidal sinus: a rare presentation. Int J Case Rep Images. 2016;7(1):48-50.1;7(1):48-50. doi:10.5348/ijcri-201610-CR-10597
- Salih AM, Mohammed SH, Dahat AH. Postauricular pilonidal sinus; a case report with literature review. Pilonidal Sinus Journal. 2017;3(1):4
- Shareef SH, Hawrami TA, Salih AM, Kakamad FH, Rahim HM, Hassan HA, Hussein DA. Intermammary pilonidal sinus: The first case series. International journal of surgery case reports. 2017;41:265-268. doi:10.1016/j.ijscr.2017.10.021
Copyright (c) 2025 The Author(s)

This work is licensed under a Creative Commons Attribution 4.0 International License.