Pediatric Adrenal Hydatid Cyst: A Case Report and Literature Review
Abstract
Introduction: Echinococcosis is a zoonotic disease that can affect various organs and tissues in the human body. However, primary adrenal hydatid cyst (AHC) is rare and may be overlooked, making its early detection crucial. This report presents a case of an incidentally diagnosed primary AHC.
Methods: A 5-year-old female with an unremarkable medical history underwent abdominal ultrasonography for assessment of an inguinal hernia, and a right adrenal lesion was incidentally discovered. Intraoperatively, the lesion was suspected to be AHC, which was later confirmed by histopathology.
Results: The 10 cases of AHC that were reviewed had a mean age of 46.2 ± 12.2 years; six patients were male. Three cases had a history of contact with animals. No laterality differences were observed, and the mean cyst size was 7.45 ± 2.7 cm. Flank pain was the most common symptom (3 of 10), and surgery was performed for all the cases, accompanied by antiparasitic drugs in five cases. No cases of recurrence were reported.
Conclusion: Primary AHC can be easily overlooked or misdiagnosed as an adrenal mass, often being identified incidentally during investigations for unrelated health concerns. Surgical excision of the cyst without rupture may yield favorable results.
Introduction
Echinococcosis is a widely recognized zoonotic disease caused by the larval form of the tapeworm Echinococcus granulosus [1]. Although the disease can occur globally, it is considered endemic in several regions, including the Middle East, the Mediterranean basin, parts of South America, South Africa, and Australia [1]. Humans serve as accidental intermediate hosts for the parasite, acquiring the infection through direct contact with definitive hosts (such as dogs) or via ingestion of food or water contaminated with feces that contain parasitic eggs, often originating from livestock environments involving sheep, goats, or cattle [2]. Major risk factors include close contact with dogs, involvement in livestock activities, and living in endemic areas [2]. The prevalence of hydatid cysts in children differs by region, with a reported incidence of 2-6 cases per 100,000 children affecting individuals as young as six months old. Human infections typically occur incidentally through the ingestion of parasite eggs in contaminated food or water or by direct contact with infected hosts [3,4]. Hydatid cysts (HCs) are typically found in the liver and lungs, while the adrenal gland is a rare and unusual site of involvement [5]. This report presents a case of a primary adrenal HC (AHC) that was incidentally diagnosed in a child. The references cited in this report have been reviewed to ensure the exclusion of any non-peer-reviewed data, and the study has been structured following the CaReL guidelines [6,7].
Case presentation
Patient information and clinical findings
A 5-year-old girl presented with a two-month history of reducible inguinal swelling on the left side. She had undergone a left inguinal herniotomy nine months earlier. The swelling, consistent with a recurrent inguinal hernia, increased in size during episodes of coughing or crying. Otherwise, her past medical history was unremarkable. She belonged to a socioeconomically poor family with limited education and resided in an urban area. Notably, her grandfather, who lived in a rural area and had direct contact with animals, had a history of HC.
Diagnostic approach
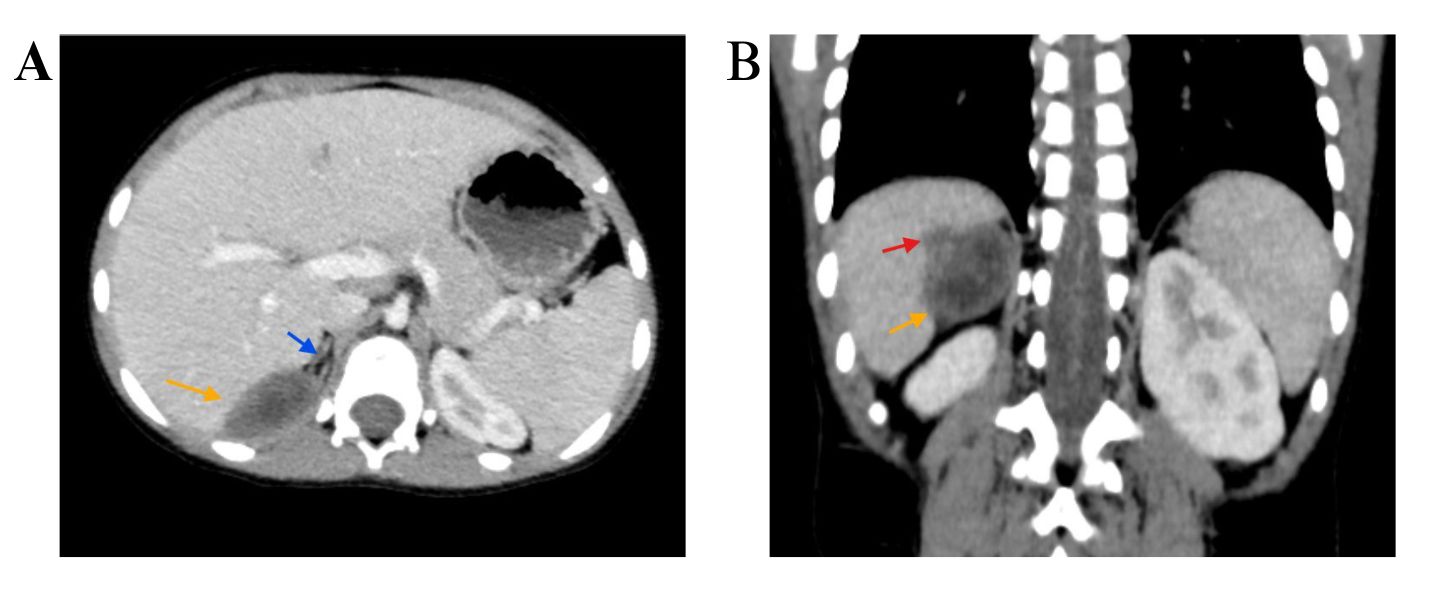
Ultrasonography was performed to rule out a right-sided inguinal hernia. Incidentally, it revealed a well-defined 30 × 20 mm lesion with a central cystic area between the right kidney's upper pole and the liver's right lobe, suggesting an adrenal lesion. Five days later, a follow-up ultrasound conducted by another radiologist identified a similar well-defined lesion measuring 31 × 19 mm. Subsequently, the patient was referred to a pediatric hematologist for further evaluation. Laboratory investigations revealed a normal complete blood count. Urinalysis indicated the presence of mucus, while aspartate aminotransferase (38 IU/L, Normal range: 15–40 IU/L) was borderline elevated, lactate dehydrogenase (370 IU/L, Normal range: 100–250 IU/L ), and erythrocyte sedimentation rate (28 mm/hr, Normal range: 0–10 mm/hr) were elevated. Computed tomography (CT) of the chest and abdomen demonstrated a well-defined, irregular, heterogeneous mass in contact with the right adrenal gland, with evidence of invasion into segment VII of the liver and involvement of the posterior right hemidiaphragm (Figure 1).
Therapeutic intervention
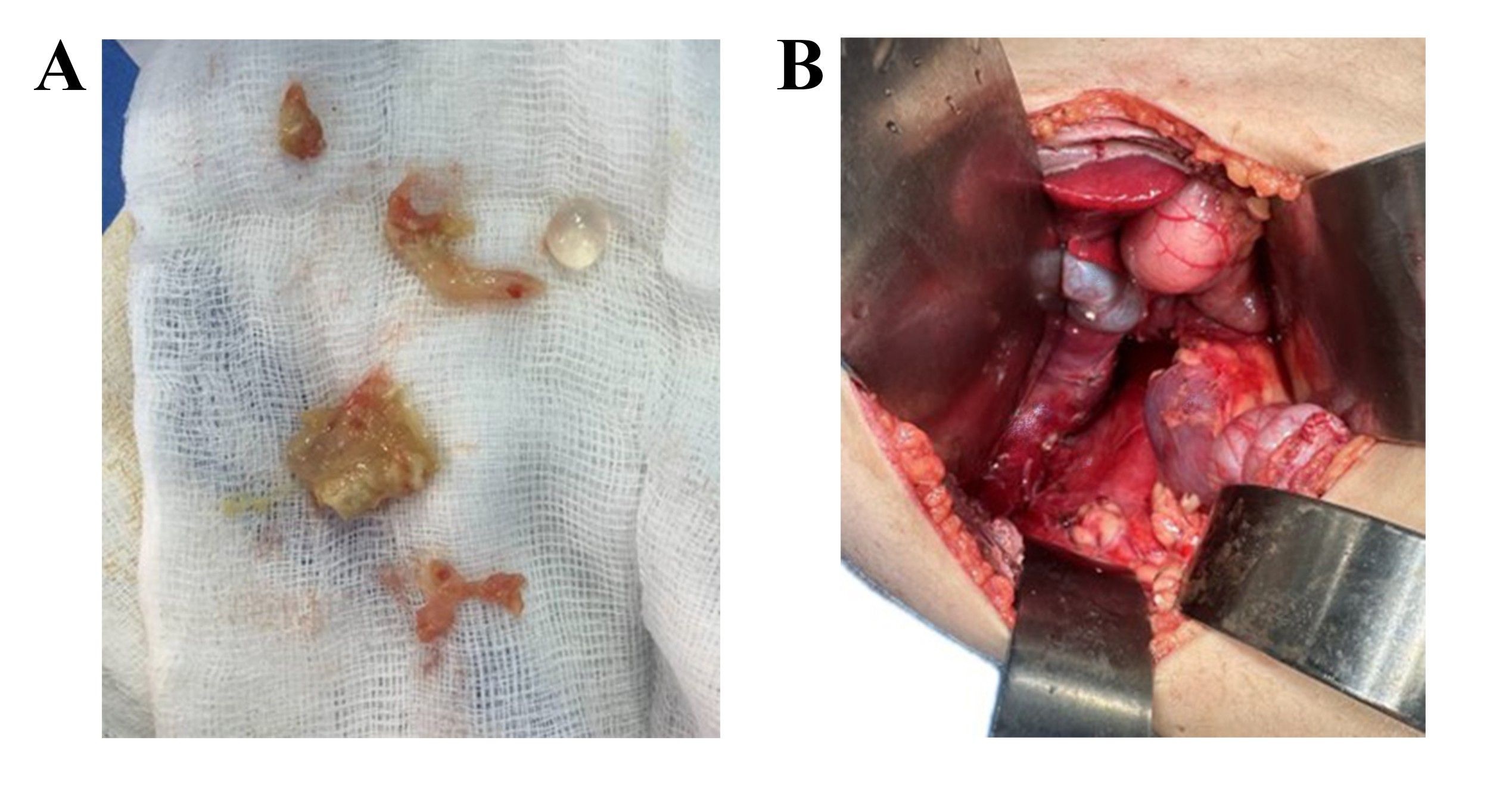
Following a multidisciplinary discussion, the patient underwent surgery under general anesthesia. The procedure involved complete resection of the mass through a 10cm right subcostal incision, along with the excision of several ipsilateral lymph nodes for histopathological analysis (Figure 2). Subsequently, a left-sided herniotomy for the recurrent hernia was performed. Albendazole was administered postoperatively.
Follow-up
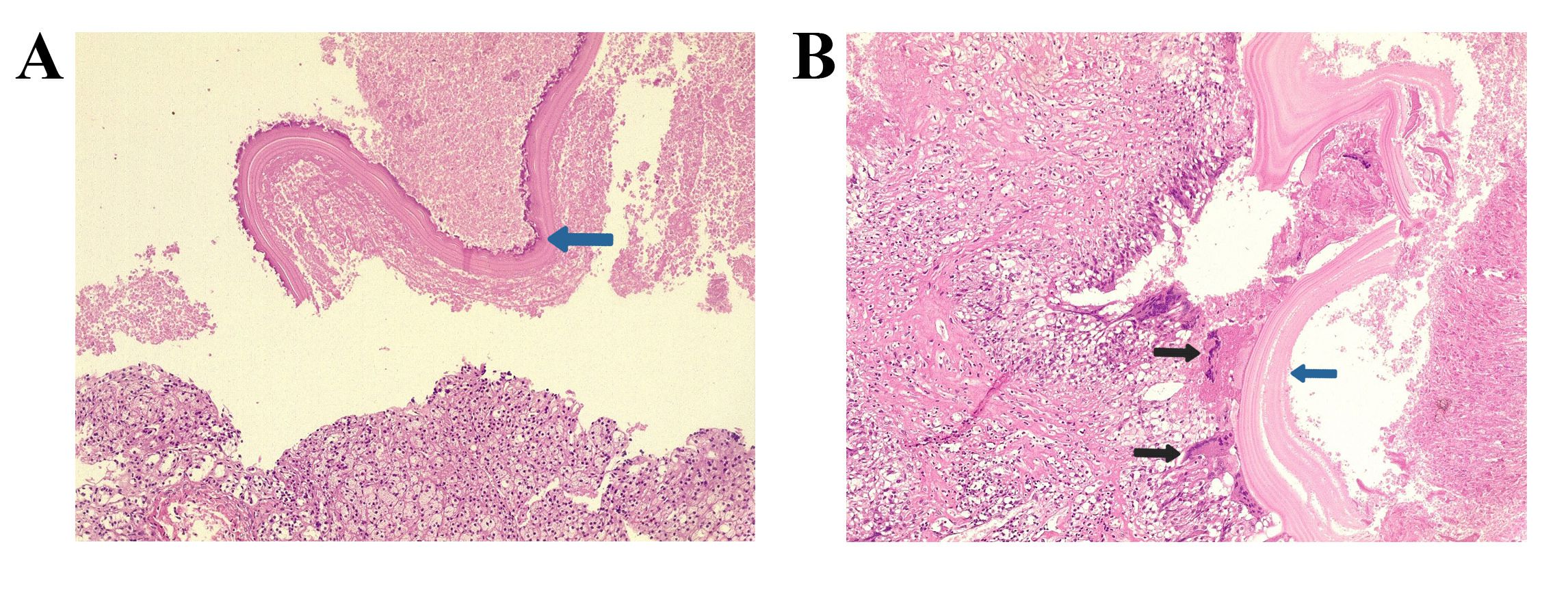
On the eighth postoperative day, the surgical wound was clean and dry. Histopathological examination revealed an infected wall of HC, accompanied by a granulomatous reaction, with adherent and compressed adrenal and liver tissue (Figure 3). Additionally, the ipsilateral lymph nodes exhibited reactive follicular hyperplasia. The patient's recovery was uneventful, and she remains under ongoing follow-up care.
Discussion
Four distinct types of Echinococcus have been recognized as responsible for hydatid disease in humans, with E. granulosus being the most commonly encountered type (95%) [8]. The disease can affect all organs and tissues in the human body [9]. The mechanism behind adrenal involvement remains unclear. The most plausible theory suggests that once the larvae exit the digestive system, they pass through the hepatic filter to reach the lungs. If they evade destruction by the immune system or are not trapped in the filtration system, they can spread out to the unusual sites of the body, such as the spleen, kidneys, brain, bones, heart, muscle tissue, pancreas, retroperitoneum, thyroid, and adrenal glands via the arterial circulation [5]. Larvae can also disseminate through systemic circulation via lymphatic vessels or direct adjacent contact [5]. AHC is a rare entity, accounting for only 0.073% of all hydatid cyst cases [9].
While individuals of all ages can be affected, this condition is more frequently seen in those aged 50 to 60, with a slightly higher prevalence in women [10]. However, the 10 reviewed cases had a mean age of 46.2 ± 12.2 years; six patients were male. The youngest case was an 18-year-old male, and the oldest was a 64-year-old male [5, 8-16]. The present case was only a 5-year-old female, which seems to be an infrequent age for this disease. Children can contract the infection through several pathways, such as direct contact with infected animals or consuming contaminated food or water. Furthermore, the higher prevalence of HCs in endemic areas accounts for the increased incidence in younger age groups.
The disease typically presents as unilateral in 92% of cases and does not exhibit a preference for either side [11]. This is supported by the fact that the disease was unilateral in all 10 cases reviewed in this report, with no differences in laterality observed (Table 1) [5, 8-16]. HCs are typically asymptomatic and often found incidentally during imaging studies for other reasons. They seldom lead to complications and usually become symptomatic primarily due to pressure-related effects [8].
|
Author /year [reference] |
Age (Y) |
Sex |
Country |
Contact with animals |
Tumor size (cm) |
Side |
Symptoms |
Medical history |
Therapeutic approach |
Recurrence |
Follow-up (M) |
|
Zouari et al./ 2020 [5] |
55 |
N/A |
Tunisia |
N/A |
12 |
Left |
Left hypochondrium pain |
None |
Surgery |
N/A |
N/A |
|
Tajmalzai et al./ 2025 [8] |
18 |
M |
Afghanistan |
Yes |
5.2 |
Right |
Right side flank pain |
None |
Albendazole & Surgery |
No |
N/A |
|
Agarwal et al./2024 [9] |
38 |
M |
India |
N/A |
6.8 |
Right |
Vague abdominal pain |
None |
Surgery & Albendazole |
No |
12 |
|
Staouni et al./ 2022 [10] |
46 |
F |
Morocco |
N/A |
6 |
Left |
Left hypochondrial pain |
None |
Surgery |
No |
12 |
|
Salih et al./ 2018 [11] |
48 |
F |
United Arab Emirates |
Yes |
7.2 |
Left |
Large palpable mass, moderate left loin pain |
None |
Laparoscopic surgery |
N/A |
N/A |
|
Tazi et al./ 2012 [12] |
64 |
M |
Morocco |
No
|
11.3 |
Left |
Left flank pain nausea & vomiting |
Arterial hypertension |
Surgery |
No |
24 |
|
Elzein et al./ 2016 [13] |
44 |
M |
Saudi Arabia |
Yes |
7.1 |
Right |
Flank pain |
N/A |
Surgery & Albendazole |
N/A |
N/A |
|
Abdulmajed et al./ 2010[14] |
48 |
F |
Turkey |
No |
5.2 |
Right |
Vague right loin pain |
Systolic hypertension |
Surgery & Albendazole |
N/A |
N/A |
|
Bouchaala et al./ 2021[15] |
46 |
M |
Tunisia |
No |
9.7 |
Right |
Non-specific abdominal pain |
Abdominal pain & weight loss |
Surgery & Albendazole |
No |
N/A |
|
Nardi et al./ 2015 [16] |
55 |
M |
Argentina |
N/A |
4 |
Left |
Back pain |
None |
Laparoscopic surgery |
N/A |
N/A |
|
M: male, F: female, N/A: non-applicable,Y: Years, M: months |
|||||||||||
The most common symptoms are pain (hypochondriac or flank pain), nausea and vomiting, and palpable mass, usually due to inflammation of adjacent tissues caused by the cyst. Systemic symptoms may also occur, such as hypertension resulting from renal artery occlusion or symptoms that mimic pheochromocytoma due to compression of the adrenal medulla by cysts [9]. The most severe complication of HCs is cyst rupture, leading to anaphylaxis and bleeding [5,10]. Flank pain was the most common presenting symptom among the reviewed cases (3 of 10), with no systemic or severe complications reported [5,8-16]. Consistent with the literature, the present case was asymptomatic, and the HC was incidentally detected as an adrenal lesion on ultrasonography performed for an inguinal hernia.
The imaging characteristics of hydatid disease vary depending on the stage of progression. Early lesions present as purely cystic, and as the germinal layer undergoes changes and intraluminal pressure decreases, the capsule becomes fibrotic and may occasionally calcify. Meanwhile, daughter cysts can detach from the wall and float within the lumen [12]. Based on the histopathological findings, which revealed a lamellated wall with cellular debris, accompanied by chronic inflammation and a foreign body giant cell reaction, the features may suggest that the cyst was in a relatively advanced or degenerative stage.
The differential diagnosis of an adrenal cyst includes an endothelial cyst, a pseudocyst caused by infarction or hemorrhage in the adrenal gland, cystic neoplasm, cystic lymphangioma, calcified hemorrhagic cyst, extra-adrenal cystic masses, and post-traumatic cysts [9]. The identification of HCs in the adrenal gland primarily relies on ultrasonography and CT scans. Ultrasound has a sensitivity of 93% to 98% for diagnosis, while CT scans achieve around 97% sensitivity [10]. Ultrasound is typically the initial examination. However, the depth of the adrenal glands and occasional peripheral calcifications can make this assessment challenging. A CT scan provides a clearer view of the location and its relationship with nearby organs [5]. Hydatid serology (such as hemagglutination and ELISA) can offer diagnostic confirmation when results are positive. However, false negative results are possible [13]. Recognizing rare presentations like adrenal involvement is clinically important to avoid misdiagnosis and utilize an appropriate therapeutic approach.
The treatment for the AHCs is primarily surgery. The two preferred options are pericystectomy and complete adrenal gland resection. However, the cyst resection while preserving the gland is considered the optimal approach [14,15]. Some authors reported that the laparoscopic approach represents a viable option due to its association with low morbidity and complication rates when performed by experienced surgeons [16]. In the present case, a CT scan was conducted following the incidental finding on ultrasonography. The scan revealed a well-defined, irregular, heterogeneous mass in contact with the right adrenal gland, with evidence of invasion into segment VII of the liver. Subsequently, the patient underwent surgery, during which the mass was completely resected. Histopathological examination confirmed the diagnosis of AHC.
Conclusion
Primary AHC can be easily overlooked or misdiagnosed as an adrenal mass, often being identified incidentally during investigations for unrelated health concerns. Surgical excision of the cyst without rupture may yield favorable results.
Declarations
Conflicts of interest: The authors have no conflicts of interest to disclose.
Ethical approval: Not applicable.
Consent for participation: Not applicable.
Consent for publication: Written informed consent for publication was obtained from the parents.
Funding: The present study received no financial support.
Acknowledgments: None to be declared.
Authors' contributions: WNS, HAY, SFA, FHK, and MMA: Major contributors to the conception of the study, as well as the literature search for related studies, and manuscript writing. SFA, HOA, BAA, and KAN: Literature review, critical revision of the manuscript, and processing of the table. PAN, SMA, and SSA: Literature review, and processing of the figures. All authors have read and approved the final version of the manuscript.
Use of AI: ChatGPT-3.5 was used to assist with language refinement and improve the overall clarity of the manuscript. All content was thoroughly reviewed and approved by the authors, who bear full responsibility for the final version.
Data availability statement: Not applicable.
References
- Rashid RJ, Tahir SH, Abid AA, Ismaeil DA, Anwar KA, Hiwa DS, Ahmad HK, Hasan AH, Sabr NS, Kakamad FH, Ahmed SM. Primary hydatid cyst of the diaphragm: A systematic review. Indian Journal of Thoracic and Cardiovascular Surgery. 2025:1-0. doi:10.1007/s12055-025-01930-x
- Pradhan E, Alrasheed SH, Melnyk OI, Azimi H, Raeisi S, Aghajani A, Ashenef B, Abdulkarim MM, Mirdan RE, Nasralla HA, Mahmood YM. Hydatid Cyst of The Orbit: A Systematic Review with Meta-Data. Barw Medical Journal. 2025;3(2). doi:10.58742/bmj.v3i2.173
- Kakamad F, Anwar KA, Ahmed HK, Habibullah IJ, Kaka Ali HH, Nasralla HA, et al. Risk Factors Associated with Human Echinococcosis: A Systematic Review and Meta-analysis. Frontiers in Veterinary Science.2024;11:1480579. doi:10.3389/fvets.2024.1480579
- Sabr WN, Hattam AS, Hasan KM, Kareem HO, Ahmed HK, Kakamad SH et al. Bilateral Giant Hydatid Pulmonary Cysts in a Pediatric Patient: A Rare Case Report. Barw Medical Journal. 2024;2(1):63-67. doi:10.58742/beb68v43
- Zouari S, Marouene C, Bibani H, Saadi A, Sellami A, Kacem LH, et al. Primary Hydatid Cyst of the adrenal gland: A case report and a review of the literature. International Journal of Surgery Case Reports. 2020 ;70:154-8. doi:10.1016/j.ijscr.2020.04.073
- Abdullah HO, Abdalla BA, Kakamad FH, Ahmed JO, Baba HO, Hassan MN, et al. Predatory Publishing Lists: A Review on the Ongoing Battle Against Fraudulent Actions. Barw Medical Journal. 2024;2(2):26-30. doi:10.58742/bmj.v2i2.91
- Prasad S, Nassar M, Azzam AY, García-Muro-San José F, Jamee M, Sliman RK, et al. CaReL Guidelines: A Consensus-Based Guideline on Case Reports and Literature Review (CaReL). Barw Med J. 2024;2(2):13-19. doi:10.58742/bmj.v2i2.89
- Tajmalzai A, Aien MT. Primary adrenal hydatid cyst: A rare entity and literature review. Radiology Case Reports. 2025 ;20(1):18-22. doi:10.1016/j.radcr.2024.09.108
- Agarwal P, Aiyer HM, Singh TP, Sharma G. A Case of a Primary Giant Adrenal Gland Hydatid Cyst—An Exceptional Location: A Case Report. Apollo Medicine. 2024 :09760016241281908. doi:10.1177/09760016241281908
- Staouni IB, El Bouardi N, Ferhi M, Haloua M, Alami BE, Lamrani YA, et al. Primary hydatid cyst of adrenal gland: Case report. Radiology Case Reports. 2022 ;17(9):3188-90. doi:10.1016/j.radcr.2022.05.084
- Salih AJ, Al-Jazeri A, Sandal M, Makki MM, Hotait H. A Large Isolated Hydatid Cyst of the Left Adrenal Gland: A Case Report–Treated by Transabdominal Laparoscopic Approach by Reflecting the Descending Colon and Review of the Literatures. Hamdan Medical Journal. 2018 ;11(2):84-6. doi:10.4103/HMJ.HMJ_12_18
- Tazi F, Ahsaini M, Khalouk A, Mellas S, Stuurman-Wieringa RE, Elfassi MJ, et al. Giant primary adrenal hydatid cyst presenting with arterial hypertension: a case report and review of the literature. Journal of Medical Case Reports. 2012 ;6:1-5. doi:10.1186/1752-1947-6-46
- Elzein FE, Aljaberi A, AlFiaar A, Alghamdi A. A Large Isolated Hydatid Cyst of the Adrenal Gland: A Case Report and Review of the Literature. Case reports in endocrinology. 2016;2016(1):9237903. doi:10.1155/2016/9237903
- Abdulmajed M, Reşorlu B, Kara C, Türkölmez K. Isolated primary hydatid cyst of adrenal gland: a case report. Turkish Journal of Urology. 2010 ;36(2):211-5. doi:10.5152/tud.2010.019
- Bouchaala H, Mejdoub I, Mseddi MA, Kammoun O, Rebai N, Slimen MH. Giant primary hydatid cyst of the adrenal gland: A rare case report. Urology Case Reports. 2021;36:101580. doi:10.1016/j.eucr.2021.101580
- Nardi W, Buero A, Lozano S, Porto EA. Laparoscopic resection of a bulky primary adrenal hydatid cyst. Journal of minimal access surgery. 2015 ;11(4):279-81. doi:10.4103/0972-9941.152103
Copyright (c) 2025 The Author(s)

This work is licensed under a Creative Commons Attribution 4.0 International License.